IIT-B develops low-cost tech to treat cancer
In a breakthrough in research, IIT-Bombay scientists have developed technology to leverage a patient’s immune system to cure cancer. Such immunotherapy using CAR T-cells, a treatment for cancer, which costs Rs 3-4 crore in US, can be made available for Rs 15 lakh, if the technology is developed in the country.
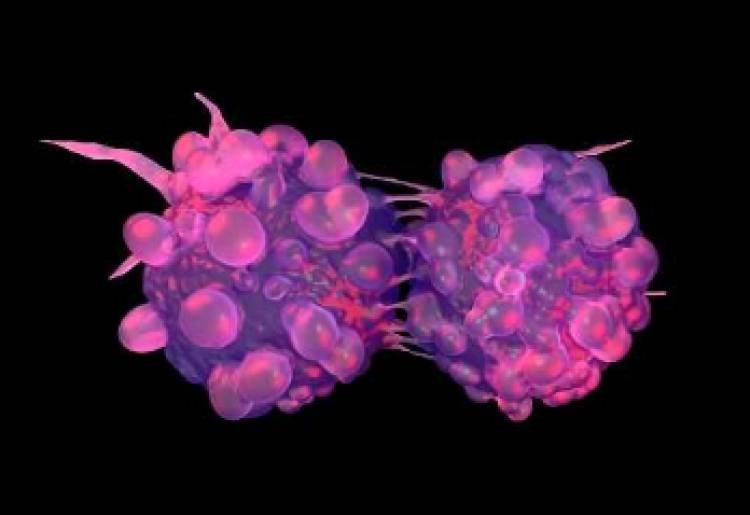
Researchers made use of gene and cell therapies to re-engineer immune cells to attack and kill cancer cells in the body. The treatment is less painful than surgery, chemotherapy or radiation, and is known to lower chances of a relapse. The therapy, which seems promising in the treatment of cancer, especially leukaemia, is currently not available in India. With the growing burden of cancer in the country, success in even a fraction of the patients using the technique will be remarkable, experts said.
Prof Rahul Purwar and his team of scientists from the institute’s Department of Biosciences and Bioengineering have conducted laboratory tests and hope to start clinical trials in collaboration with Dr Gaurav Narula from Tata Memorial Hospital (TMH) next year, after getting permission from Drug Controller General of India (DCGI). A facility has been created for it at the hospital’s Kharghar campus.
T-cells (type of white blood cell or WBC), an integral part of the human immune system, can identify tumours and destroy them. But in advanced stages, the cancer cells adapt to the presence of T-cells and remain undetected. In the new approach in immunotherapy, called CAR (chimeric antigen receptors) T-cell therapy, the T-cell’s ability to detect and kill cancer cells is restored. CARs are protein that assist T-cells to recognise and attach to protein or antigen, present on cancer cells. These proteins help destroying cancer cells.
Purwar’s team has been working on CAR T-cell technology for six years. “It is an autologous cell therapy for personalised medicine, where cells are taken from patients, re-engineered and re-infused in the patient. We got immune cells from volunteers and clinical patients with help from TMH and re-engineered them using the technique. The modified cells were positively tested in laboratories on artificially grown cancer cells,” said Purwar.
“Our team has delved into strategies that would improve efficacy of the technique and demonstrated that a single injected dose can lead to multiplication of modified T-cells that can destroy cancer cells,” said Purwar.
A private firm is planning to in-licence the technology and is trying to make the therapy available for Indian patients for about Rs 35 lakh. Purwar and two researchers are working on the technology as part of their start-up ImmunoAdaptive Cell Therapy or ImmunoACT, which was incubated at IIT-Bombay.
Globally, over 600 clinical trials are in progress for CAR T-cell therapy, many of which are on in China, said Dr Narula from TMH. “It has got huge potential. With the cancer burden we have, the therapy will be considered a success, even if it applicable to only a fraction of patients currently. Technologies are being developed globally, but are exorbitant. The only way to cut costs is by developing the technology in India, which is why we have teamed up with IIT-B about four and a half years ago, long before the first therapy was approved for clinical use in US. There are high expectations from this technology as it can create pathways for developing newer technologies, for newer therapies, for more forms of cancer,” said Narula.